If you’re tired of being tired, lying awake drenched in sweat wondering if you’ll ever sleep through the night again, this is your rescue plan.
The Sleep Crisis of Perimenopause
For most of my life, sleep has been like shifting sand. Sometimes solid, sometimes slipping out from under me. As a teen, I wasn’t consuming much sugar—and later cut it out completely—but I still wrestled with blood sugar swings, late-night restlessness, and an over-revved nervous system. Looking back, I can see it wasn’t really about sugar at all. Chronic stress and hidden inflammation were already pushing my cortisol out of rhythm, keeping my body on high alert when it should have been at rest. I knew early on that gluten wasn’t my friend, but it took me until college to take it seriously. In those years, I even pushed myself to exercise until exhaustion, just so I could finally fall asleep.
Fast-forward to perimenopause: sleep disruptions look different, but they’re just as real. These days, it’s less about my body being revved up and more about the practical realities of life — a nursing toddler who still wakes in the night, or my tendency to steal quiet hours for productivity once everyone else is asleep. And then there are those occasional 2 a.m. wake-ups to use the loo. My body is much less stressed than it once was, but the cracks in sleep still show.
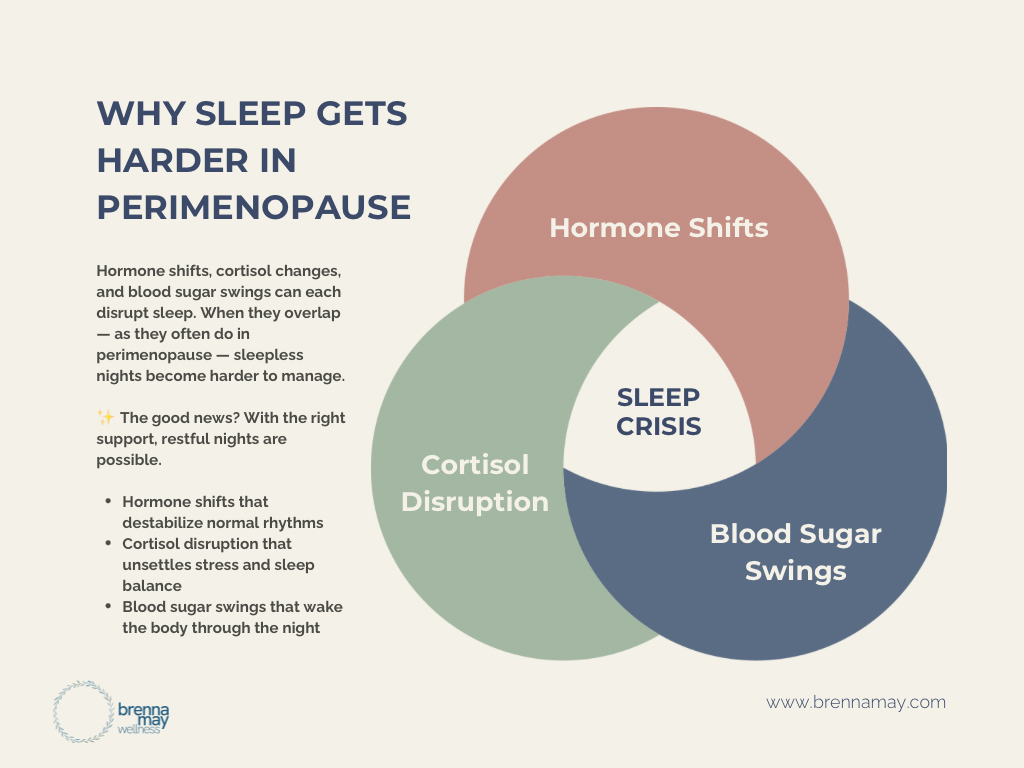
And I’m far from alone. Research shows that sleep disruption is one of the most common symptoms of perimenopause, reported by up to 61% of women (Joffe et al., 2010, PMID: 20606998). It isn’t just about feeling tired the next day, either. Poor sleep amplifies hot flashes, fuels anxiety, worsens autoimmune flares, and erodes resilience in every system of the body (Kravitz et al., 2008, PMID: 19061818). In fact, sleep researchers call the menopausal transition a “perfect storm” for insomnia, combining hormonal shifts, vasomotor symptoms, and altered cortisol rhythms into one exhausting package (Baker et al., 2018, PMID: 30098788).
Such is the sleep crisis of perimenopause. If you’ve found yourself lying awake at 3 a.m., drenched in sweat, your mind racing, wondering if you’ll ever get a solid night of sleep again—you are not broken. You’re living through one of the most biologically disruptive times in a woman’s life. And the good news? There are natural, proven ways to restore peace to your nights.
Rest and Peace Are Non-Negotiable Foundations
One of the hardest lessons I’ve learned is this: you can’t run on empty forever. For years, I believed that pushing through meant strength. But in reality, sleep is the scaffolding that holds up everything else—hormone balance, blood sugar regulation, mental clarity, even emotional resilience. Without it, everything crumbles.
In perimenopause, this truth becomes unavoidable. Rest and peace aren’t luxuries you’ll get around to when the laundry is folded or when the toddler sleeps through the night. They are non-negotiable foundations. If your sleep is on shifting sand, everything built on top of it—your immune system, your energy, your sanity—feels shaky. Rebuilding sleep is like laying down bedrock where your body can finally exhale.
The Science of Perimenopausal Sleep Disruption
Perimenopause brings hormonal changes that shake the stability of sleep:
- Estrogen & Progesterone: Progesterone has a calming, sleep-promoting effect. As levels drop, so does that natural sedation. Estrogen influences serotonin and melatonin, meaning dips can destabilize your sleep-wake cycle. What once felt steady starts to shift under your feet.
- Temperature Regulation: Hot flashes and night sweats—caused by fluctuating estrogen—disrupt the brain’s thermostat. Even small changes in body temperature can wake you.
- Cortisol Patterns: Cortisol, your stress hormone, naturally peaks in the morning and dips at night. But in perimenopause, stress, inflammation, or blood sugar swings can flip this rhythm, leaving you awake at 2 a.m. with your body acting like it’s daytime.
The Night Sweat Solution
Vasomotor symptoms—those sudden waves of heat and sweating—are one of the most disruptive parts of perimenopausal sleep. But there are simple, practical steps that help:
- Cool the environment: Keep your room 60–67°F (15–19°C). A fan or cooling natural latex mattress pad can make all the difference.
- Choose breathable layers: Light cotton or moisture-wicking sleepwear helps regulate temperature. Layer bedding so you can peel back instead of waking in a sweat puddle.
- Reduce triggers: Alcohol, caffeine, and spicy foods close to bedtime can worsen night sweats.
Stable temperature gives your body back the firm ground it’s craving.
Natural Sleep Restoration Protocol
Restoring sleep in perimenopause means supporting your biology, not fighting it.
- Circadian rhythm support: Anchor your mornings with sunlight exposure. This helps reset melatonin release at night.
- Magnesium glycinate: Taken in the evening, this form of magnesium calms the nervous system and promotes deeper sleep.
- Adaptogenic herbs: Ashwagandha (for some), holy basil, or reishi can help regulate stress response and smooth cortisol spikes.
- Progesterone support: For some women, bioidentical progesterone under the guidance of a practitioner can restore the calming effect that’s been lost.
Sleep Hygiene for Autoimmune Women
If you live with an autoimmune condition, the stakes are higher. Inflammation worsens with poor sleep, and poor sleep worsens inflammation—a vicious loop. Try these:
- Blue light boundaries: Shut off screens 1–2 hours before bed, or use blue-blocking glasses.
- Evening nervous system care: Think bath, stretching, or prayer/meditation instead of email catch-up.
- Morning light exposure: Just 10 minutes of real daylight in the morning reinforces your circadian rhythm.
When to Seek Functional Testing
If your sleep struggles feel insurmountable, it may be time to look deeper. Functional testing can reveal the underlying “why”:
- Cortisol rhythm testing (like a DUTCH test): Shows whether stress hormones are spiking at night.
- Hormone panels: Reveal if progesterone or estrogen dips are driving your symptoms.
References
- Joffe, H., et al. (2010). Sleep disturbance during the menopausal transition. Sleep Med Clin 5(1):33-43. PMID: 20606998
- Kravitz, H.M., et al. (2008). Sleep during the perimenopause: a SWAN story. Obstet Gynecol Clin North Am 35(4):567-576. PMID: 19061818
- Baker, F.C., et al. (2018). Sleep and Sleep Disorders in the Menopausal Transition. Sleep Med Clin 13(3):443-456. PMID: 30098788
If perimenopause has left you feeling like restful sleep is a luxury, remember this: your body is not fighting against you—it’s asking for deeper care. Rest and peace aren’t indulgences, they’re foundations. With the right rhythms, tools, and environment, your nights can once again become a place of healing rather than struggle.
✨ You’ll find gentle, professional-grade sleep support — like magnesium glycinate, calming adaptogens, and nervine blends — in my Fullscript Dispensary.
For tailored support in navigating perimenopause, apply to work with me.
Brenna May, NTP
Holistic Nutritional Therapy Practitioner • Functional Wellness
This content is for educational purposes only and is not a substitute for individualized medical advice.
Next up: Energy Reset in Perimenopause